Endothelial Protection
Cardiovascular mortality in dialysis patients is 10–20 times higher than in the general population and seems to be more than 100 times higher in patients younger than 45 years of age (1). The etiology of cardiovascular disease in end stage kidney disease (ESKD) patients is complex and multifactorial; volume and pressure overload, abnormalities in cardiac morphology and function, dyslipidemias, atherosclerosis, and nutritional derangements all play a role.
At the heart of atherosclerosis is an abnormal and dysfunctional endothelium. Bone marrow-derived endothelial progenitor cells (EPCs) are important for endothelial maintenance. EPCs mediate repair of damaged vascular endothelium, promote angiogenesis, and protect the blood vessel from atherosclerosis development (2). Several reports in the literature describe qualitative and quantitative abnormalities of EPCs in uremic and dialyzed patients (3–7).
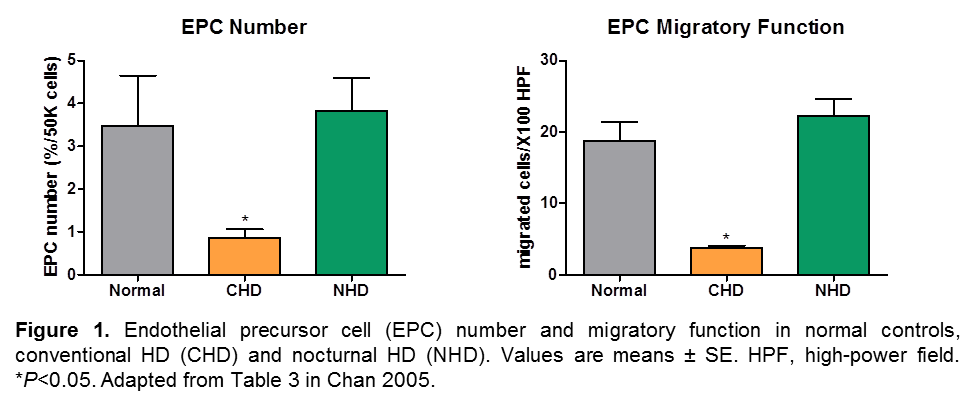
Intensifying the hemodialysis (HD) prescription does not appear to have a direct effect on endothelial progenitor cell numbers; however, Chan et al. hypothesized that improved uremic toxin removal during daily, nocturnal hemodialysis can result in improved EPC number and function, improving overall cardiovascular parameters in dialysis patients. EPCs were isolated from 3 groups of age- and gender-matched subjects (normal control, n=10; conventional, thrice weekly HD (CHD), n=12; and daily, nocturnal HD, n=10 patients) (8). None of the patients had symptomatic cardiovascular disease. EPC function was assessed by in vitro testing of the migratory response to 50 ng/mL of vascular endothelial growth factor. Left ventricular mass index (LVMI) was derived using 2D echocardiography. EPC number and function were markedly impaired in CHD patients despite higher doses of erythropoietin. In contrast, nocturnal HD (NHD) patients had similar EPC biology to normal controls (Figure 1). EPC number and function inversely correlated to pre-dialysis urea concentration and LVMI.
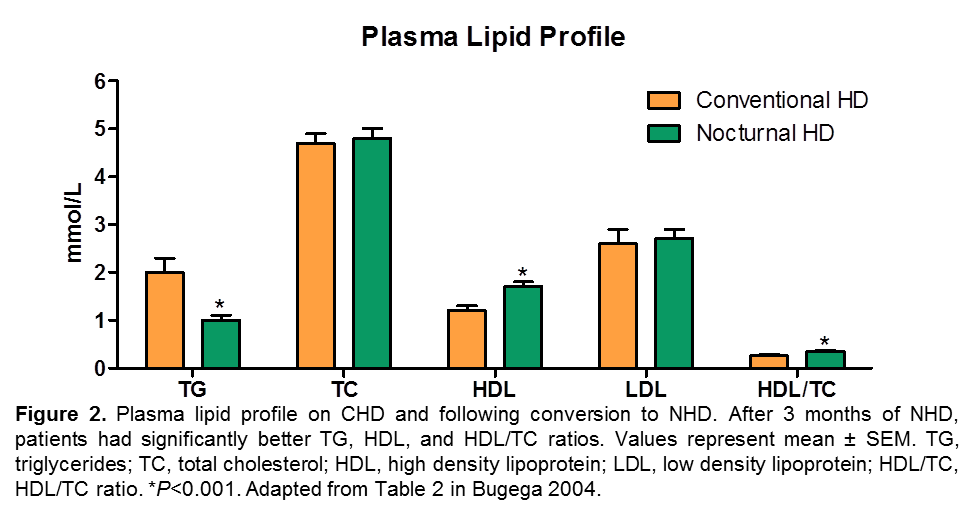
In addition to EPC parameters, a number of papers have described improvement in dyslipidemia with intensified hemodialysis. Since this also could not be a direct effect, it is assumed that intensified HD better removes one or more solutes that impairs normal lipid metabolism. Bugeja et al. conducted a prospective cohort study of 11 ESRD patients before and after conversion from conventional to daily (5-6 times/week) nocturnal hemodialysis (9). A 12-hour fasting lipid profile was obtained while on CHD and after 3 months on stable NHD. Three months after conversion from CHD to NHD, a significant fall in serum triglycerides associated with a significant rise in HDL-cholesterol and HDL/total cholesterol ratio was identified as shown in Figure 2. Total cholesterol and LDL cholesterol were unchanged. Although changes of this magnitude in lipid profile might be considered as a clinically significant response to any other lipid lowering therapy, it must be noted that randomized controlled trials with lipid lowering drugs (statins) have not shown any improvement in clinical outcomes in patients on maintenance HD (10,11).
Reference:
- Foley RN, Parfrey PS, Sarnak MJ. Epidemiology of cardiovascular disease in chronic renal disease. J Am Soc Nephrol. 1998;9(12 Suppl):S16-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11443763.
- Hill JM, Zalos G, Halcox JPJ, Schenke WH, Waclawiw MA, Quyyumi AA, Finkel T. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003;348(7):593-600. Available from: http://www.ncbi.nlm.nih.gov/pubmed/12584367.
- Bahlmann FH, DeGroot K, Duckert T, Niemczyk E, Bahlmann E, Boehm SM, Haller H, Fliser D. Endothelial progenitor cell proliferation and differentiation is regulated by erythropoietin. Kidney Int. 2003;64(5):1648-1652. Available from: http://www.ncbi.nlm.nih.gov/pubmed/14531796.
- Chen Y-LY-T, Cheng B-C, Ko S-F, Chen C-H, Tsai T-H, Leu S, Chang H-W, Chung S-Y, Chua S, Yeh K-H, et al. Value and level of circulating endothelial progenitor cells, angiogenesis factors and mononuclear cell apoptosis in patients with chronic kidney disease. Clin Exp Nephrol. 2013;17(1):83-91. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22814956.
- Jourde-Chiche N, Dou L, Sabatier F, Calaf R, Cerini C, Robert S, Camoin-Jau L, Charpiot P, Argiles A, Dignat-George F, et al. Levels of circulating endothelial progenitor cells are related to uremic toxins and vascular injury in hemodialysis patients. J Thromb Haemost. 2009;7(9):1576-1584. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19583820.
- Krieter DH, Fischer R, Merget K, Lemke H-D, Morgenroth A, Canaud B, Wanner C. Endothelial progenitor cells in patients on extracorporeal maintenance dialysis therapy. Nephrol Dial Transplant. 2010;25(12):4023-4031.
- Kun-Ying Z, Hui-Lan L, Xiao-Feng D, Guo-Gang L. Association between Circulating Endothelial Cells and Carotid Atherosclerosis in Patients Receiving Maintenance Hemodialysis. 2014. Available from: http://dx.doi.org/10.1155/2014/753759.
- Chan CT, Li SH, Verma S. Nocturnal hemodialysis is associated with restoration of impaired endothelial progenitor cell biology in end-stage renal disease. Am J Physiol Renal Physiol. 2005;289(4):F679-84. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15928211.
- Bugeja AL, Chan CT. Improvement in lipid profile by nocturnal hemodialysis in patients with end-stage renal disease. ASAIO J. 2004;50(4):328-331. Available from: http://www.ncbi.nlm.nih.gov/pubmed/15307542.
- Wanner C, Krane V, März W, Olschewski M, Mann JFE, Ruf G, Ritz E. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med. 2005;353(3):238-248. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16034009.
- Fellström BC, Jardine AG, Schmieder RE, Holdaas H, Bannister K, Beutler J, Chae D-W, Chevaile A, Cobbe SM, Grönhagen-Riska C, et al. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N Engl J Med. 2009;360(14):1395-1407. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19332456.
P/N 102559-01 Rev B 05/2021
