Treatment
Empiric antibiotic therapy can be started immediately, or treatment can be delayed pending culture results. Empiric therapy should at least cover Staphylococcus aureus (1).
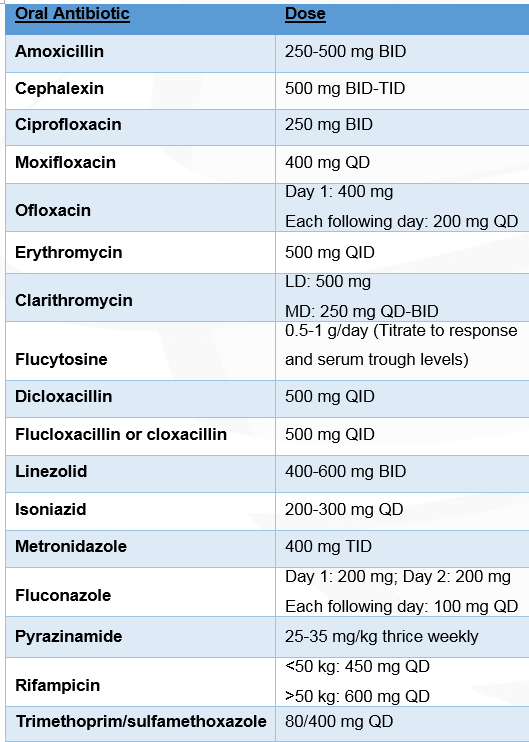
Adapted from: Li PK-T, et al. Peritoneal dialysis-related infections recommendations: 2010 update. Perit Dial Int. 30(4):393-423.
Abbreviations: BID: Twice daily; TID: Three times daily; QD: Every day; QID: Four times daily
Treatment with oral antibiotics is preferred in patients with bacterial exit-site infections, with the exception of those caused by methicillin-resistant S. aureus (MRSA). This antibiotic therapy should be continued for at least two weeks; however treatment should continue until the exit site appearance normalizes. Rifampicin may be used in cases where exit-site infections (ESIs) caused by S. aureus are very slowly resolving; however, this agent should not be used as monotherapy due to the risk of contributing to resistance. The use of vancomycin should be reserved for infections caused by MRSA, as resistance to vancomycin may develop as well(1). When antibiotics do not resolve an ESI, complete removal of the superficial cuff, or cuff-shaving, can be performed(3).
Treatment of mild or equivocal ESIs has been successful with topical antibiotics; however, these are of limited utility in cases where profuse drainage is present(4–7). In addition, topical antibiotic therapy may not be adequate for acute or chronic active ESIs(8). Sodium hypochlorite, dilute hydrogen peroxide, 0.9% saline solution, and povidone iodine may be used as soaking solutions(4,9). Exit-site care protocols that combine the use of a topical antibiotic with an antiseptic, such as sodium hypochlorite, may also prove effective in reducing the incidence of ESIs(10). Care of the infected exit site should occur once or twice daily. Forcibly removing scabs or crusts is discouraged. Instead, soften them using soap and water, hydrogen peroxide, saline, or an exit site soak. Additionally, proud flesh may need to be cauterized to expedite the healing process(11). Nonocclusive sterile dressings are applied to absorb drainage, protect from microorganisms, and prevent trauma to the site(8,9).
When a cuff, exit site, or tunnel infection is associated with peritonitis caused by the same microorganism, catheter removal should be considered, unless the organism is Staphylococcus epidermidis. While antibiotic use may clear the effluent, the culture often remains positive leading to recurrent peritonitis until removal of the source catheter occurs. The catheter is also typically removed in refractory or recurrent peritonitis with exit or tunnel infections, as well as in extensive cellulitis that is unresponsive to antibiotic treatment. Early catheter removal is necessary in cases of fungal ESIs or in pseudomonal ESIs that fail to respond to antibiotic therapy and shaving of the external cuff(1).
References
- Li PK-T, Szeto CC, Piraino B, Bernardini J, Figueiredo AE, Gupta A, Johnson DW, Kuijper EJ, Lye W-C, Salzer W, et al. Peritoneal dialysis-related infections recommendations: 2010 update. Perit Dial Int. 2010;30(4):393-423. Available from: https://www.ncbi.nlm.nih.gov/pubmed/20628102.
- Piraino B, Bailie GR, Bernardini J, Boeschoten E, Gupta A, Holmes C, Kuijper EJ, Li PK-T, Lye W-C, Mujais S, et al. Peritoneal dialysis-related infections recommendations: 2005 update. Perit Dial Int. 2005;25(2):107-131. Available from: https://www.ncbi.nlm.nih.gov/pubmed/15796137.
- Scalamogna A, De Vecchi A, Maccario M, Castelnovo C, Ponticelli C. Cuff-shaving procedure. A rescue treatment for exit-site infection unresponsive to medical therapy. Nephrol Dial Transplant. 1995;10(12):2325-2327. Available from: https://www.ncbi.nlm.nih.gov/pubmed/8808234.
- Khanna R, Krediet RT, eds. Nolph and Gokal’s Textbook of Peritoneal Dialysis. 3rd ed. New York: Springer Science+Business Media; 2009.
- McQuillan RF, Chiu E, Nessim S, Lok CE, Roscoe JM, Tam P, Jassal SV. A randomized controlled trial comparing mupirocin and polysporin triple ointments in peritoneal dialysis patients: the MP3 Study. Clin J Am Soc Nephrol. 2012;7(2):297-303. Available from: https://www.ncbi.nlm.nih.gov/pubmed/22134627.
- Khandelwal M, Bailey S, Izatt S, Chu M, Vas S, Bargman J, Oreopoulos D. Structural changes in silicon rubber peritoneal dialysis catheters in patients using mupirocin at the exit site. Int J Artif Organs. 2003;26(10):913-917. Available from: https://www.ncbi.nlm.nih.gov/pubmed/14636007.
- Bernardini J, Bender F, Florio T, Sloand J, Palmmontalbano L, Fried L, Piraino B. Randomized, double-blind trial of antibiotic exit site cream for prevention of exit site infection in peritoneal dialysis patients. J Am Soc Nephrol. 2005;16(2):539-545. Available from: https://www.ncbi.nlm.nih.gov/pubmed/15625071.
- Burkart J, Bleyer AJ. Tunnel and peritoneal catheter exit site infections in continuous peritoneal dialysis. UpToDate. 2016.
- Piraino B, Bernardini J, Bender FH. An analysis of methods to prevent peritoneal dialysis catheter infections. Perit Dial Int. 28(5):437-443. Available from: https://www.ncbi.nlm.nih.gov/pubmed/18708532.
- Chua AN, Goldstein SL, Bell D, Brewer ED. Topical mupirocin/sodium hypochlorite reduces peritonitis and exit-site infection rates in children. Clin J Am Soc Nephrol. 2009;4(12):1939-1943. Available from: https://www.ncbi.nlm.nih.gov/pubmed/19820132.
- Prowant BF. Nursing interventions related to peritoneal catheter exit-site infections. Adv Ren Replace Ther. 1996;3(3):228-231. Available from: https://www.ncbi.nlm.nih.gov/pubmed/8827202.
P/N 103094-01 Rev A 07/2016